Behavioural activation: Re-engaging With Life When Living With Chronic Pain
Joon Choi, Clinical Psychologist
Persistent pain affects more than the body. It influences mood, motivation, daily routines, and how people participate in activities that matter to them (Nicholas, Costa & Hancock, 2023). Over time, many individuals notice that their world becomes smaller. They withdraw from social situations, physical tasks, and enjoyable activities. This pattern, although understandable, can inadvertently reinforce both pain and low mood (Lee et al., 2021).
Behavioural activation is a psychological strategy that helps people gradually re-engage with meaningful activity in a planned and sustainable way. Behavioural activation is an important psychological treatment strategy and is commonly included as part of a comprehensive pain management program. This blog outlines how behavioural activation works and why it can be an important tool for people living with persistent pain.
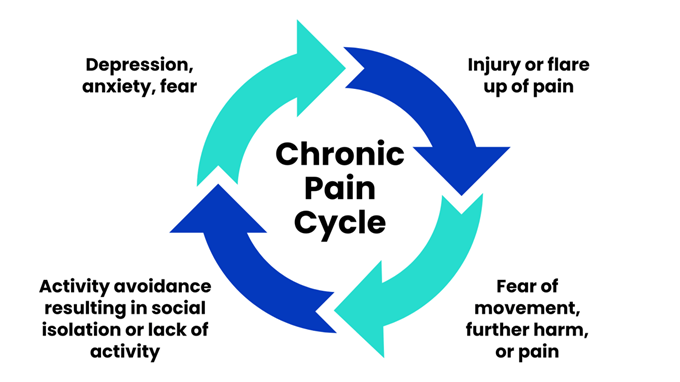
Understanding the pain–mood–activity cycle
Persistent pain often leads to reduced activity. This may begin with avoiding tasks that increase symptoms but can gradually extend to other areas of life. Reduced activity can lead to:
Lower mood
Increased fatigue
Reduced fitness and mobility
Decreased confidence
Greater focus on pain
These changes can make pain feel more intense and more limiting. The result is a cycle of pain, low mood, and avoidance that sustains itself over time. Behavioural activation aims to interrupt this cycle by using structured activity planning to rebuild confidence, mood, and function.
What is behavioural activation?
Behavioural activation is an evidence-based psychological approach originally developed for depression (Donaldson, Lamont & McMillan, 2022). It focuses on increasing engagement in activities that are meaningful, enjoyable, or create a sense of achievement. The principle is simple: mood improves when people participate in valued activities, and mood declines when activity levels drop.
In the context of persistent pain, behavioural activation helps individuals:
Understand avoidance patterns
Identify meaningful goals
Break tasks into manageable steps
Rebuild daily structure and routine
Improve mood and energy
Increase physical and social engagement
Gradually reduce disability
Importantly, behavioural activation does not require “pushing through pain”. Instead, it uses graded, consistent activity that matches an individual’s capacity and gradually expands over time.
Why avoidance increases pain over time
Avoidance is a natural response to discomfort. For short-term injuries, rest helps healing. For persistent pain, however, long periods of rest or inactivity can reduce conditioning and increase sensitivity in the nervous system (Ellingson et al., 2012). This can make even small tasks feel more painful.
People often describe two common patterns.
Boom-and-bust pattern
On a good day, they attempt to “catch up,” doing too much at once. This leads to a flare-up, followed by several days of reduced activity. Over time, this creates instability in mood and routine
Increasing avoidance
Activities once considered manageable are postponed or removed altogether. Although avoidance reduces discomfort temporarily, it reinforces the belief that pain signals danger, which can contribute to ongoing disability
Behavioural activation helps stabilise activity across the week and rebuild confidence safely.
How behavioural activation helps
Identifying what matters
Behavioural activation starts by identifying important life areas, such as family, work, leisure, health, or independence. Understanding what is meaningful provides direction for goal setting
Using micro-goals
Large tasks can feel overwhelming. Behavioural activation breaks them into small, achievable steps. Examples include:
Walking for two minutes
Doing one load of washing
Sitting outside for fresh air
Calling a friend
Preparing a simple meal
Success with small goals builds momentum and confidence
Increasing pleasant and mastery activities
Behavioural activation balances different types of activities
Pleasant activities (e.g. listening to music, reading, hobbies) support mood
Mastery activities (e.g. completing household tasks, work-related tasks) build confidence
Both are important for people with persistent pain
Rebuilding daily structure
A predictable routine helps regulate mood, sleep, and energy. Behavioural activation supports patients in creating a weekly schedule that includes self-care, rest, activity, and pacing
Supporting pacing and graded activity
Behavioural activation complements pacing principles by encouraging steady, consistent activity rather than fluctuating between overactivity and rest
Strengthening identity and quality of life
Over time, re-engaging with valued activities helps people reconnect with roles, relationships, and goals that may have been overshadowed by pain
Integrating behavioural activation within pain management
Within the pain management program, behavioural activation is often combined with:
Pain education
Physiotherapy and graded exercise
Psychological strategies for managing worry or low mood
Pacing and activity planning
Goal setting
Support around return-to-work
This multidisciplinary structure helps people understand their pain, improve daily functioning, and gradually re-engage with meaningful aspects of life (Kamper et al., 2015).
Summary
Behavioural activation is a practical and effective strategy for people living with persistent pain. By focusing on small, meaningful steps and consistent routines, individuals can regain a sense of control, improve mood, and expand their daily activities. Change is often gradual, but over time, behavioural activation can make a significant difference in quality of life and functional capacity.
References
Donaldson, L., Lamont, E., & McMillan, D. (2022). Behavioural activation for chronic pain: A systematic review and meta-analysis. Pain Medicine, 23(3), 542–553.
Ellingson, L. D., Stegner, A. J., & Cook, D. B. (2012). Physical activity and chronic pain: Mechanisms and interventions. Current Pain and Headache Reports, 16(2), 189–198.
Kamper, S. J., Apeldoorn, A. T., Chiarotto, A., Smeets, R. J., Ostelo, R. W., Guzman, J., & van Tulder, M. W. (2015). Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database of Systematic Reviews, 2015(9), CD000963.
Lee, H., Hübscher, M., Moseley, G. L., Kamper, S. J., Traeger, A. C., Mansell, G., & McAuley, J. H. (2021). How does pain lead to disability? A systematic review and meta-analysis of the role of avoidance. Pain, 162(10), 2479–2486.
Nicholas, M. K., Costa, L. d. C. M., & Hancock, M. J. (2023). Managing chronic pain: A clinical update. BMJ, 381, e073496.
Joon completed his Clinical Psychology training in New Zealand and has wide-ranging experience working in health, forensic and community settings across a number of different population groups. This has involved clinical roles in assessment and therapy, both as a lead clinician and as part of a wider multi-disciplinary team.