Sleep and Pain
Joon Choi, Clinical Psychologist
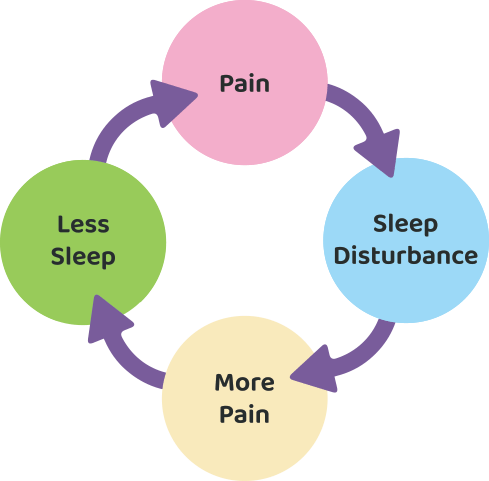
Poor sleep is often an issue that many of those with chronic pain experience. Pain can disrupt sleep, and in turn, this lack of sleep can heighten sensitivity to pain, resulting in a cycle that negatively impacts both physical and mental well-being. Improving sleep for those with chronic pain requires a multi-factorial approach that addresses both the physical and psychological factors that contribute to sleep difficulties.
Link between pain and sleep
Chronic pain often makes it difficult for individuals to fall asleep and stay asleep. Studies show that about 50-80% of people with chronic pain experience sleep problems, including insomnia, frequent awakenings, and non-restorative sleep (Whale and Gooberman-hill, 2022). This disruption in sleep patterns is largely due to the body’s response to pain. Pain is not just a physical sensation, however; it involves a complex interaction of the nervous system, brain, and emotional states.
When a person experiences pain, the brain's ability to initiate and maintain sleep is compromised. Pain can activate stress hormones, such as cortisol, which keep the body in a heightened state of alertness, making it harder to relax and fall asleep (Ulrich-Lai and Herman, 2009).
Conversely, poor sleep exacerbates chronic pain. Research indicates that sleep deprivation increases sensitivity to pain by affecting the brain’s ability to regulate pain perception (Kourbanova et al., 2022). When sleep is inadequate, the body's ability to produce anti-inflammatory proteins and repair tissues is diminished, which can worsen pain symptoms. As a result, a person trapped in this cycle of pain and poor sleep experiences more intense pain during the day and finds it even more difficult to sleep at night.
Psychological factors that can impact on sleep in chronic pain
In addition to the physical aspects of pain, psychological factors play a significant role in sleep disturbances. Chronic pain is often associated with anxiety, depression, and stress, all of which can interfere with sleep (Jennifer, 2024). Anxiety about pain worsening during the night, fears of waking up in pain, or worries about the long-term consequences of chronic pain can lead to hyperarousal—a state where the mind is too active to allow for restful sleep. Depression, a common comorbidity in people with chronic pain, is also linked to insomnia and poor sleep quality. This emotional distress not only makes it harder to fall asleep but also reduces the overall quality of sleep, preventing the deep, restorative phases of sleep that are crucial for healing.
Moreover, individuals with chronic pain may develop maladaptive behaviours and thought patterns related to sleep. For instance, they may start associating bedtime with the anticipation of pain or the frustration of being unable to sleep, which can create a negative sleep environment. This psychological conditioning can make it even more challenging to achieve restful sleep, even when physical pain is not at its peak.
Strategies for improving sleep in chronic pain
Improving sleep for those with chronic pain requires a comprehensive approach that targets both physical pain and psychological barriers to sleep. Here are several strategies that can help enhance sleep quality in individuals with chronic pain:
Pain management techniques
Proper pain management is essential for improving sleep. However, it is important to consult your doctor as part of the pain management program to ensure that these medications do not interfere with sleep patterns. Some pain medications, especially opioids, can disrupt sleep and lead to non-restorative sleep.
Graded exercise program as directed by your physiotherapist in the pain management program. Engaging in physical therapy or gentle stretching exercises can help alleviate pain and promote relaxation before sleep.
Cognitive Behavioural Therapy for Insomnia (CBT-I)
Cognitive Behavioural Therapy for Insomnia (CBT-I) is an evidence-based psychological intervention that addresses the thoughts and behaviours contributing to sleep disturbances. CBT-I helps individuals with chronic pain reframe negative thoughts about sleep and pain, replacing them with more adaptive and positive beliefs.
By addressing the psychological component of sleep problems, CBT-I can break the cycle of pain-related insomnia and improve overall sleep quality.
CBT-I also includes sleep hygiene practices, such as establishing a consistent sleep schedule, limiting naps during the day, and creating a calming bedtime routine. By reinforcing healthy sleep behaviours, CBT-I helps individuals improve their sleep patterns over time.
Relaxation techniques
Relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, meditation, and mindfulness, can help reduce tension and promote a calm mental state before bedtime. Mindfulness practices have been shown to reduce the perception of pain and improve sleep quality by helping individuals focus on the present moment rather than ruminating on pain or sleep difficulties.
Incorporating relaxation exercises into a bedtime routine can help activate the parasympathetic nervous system, which promotes relaxation and prepares the body for sleep.
Sleep environment
Creating a comfortable sleep environment is crucial for individuals with chronic pain. It may also be important to adjust the bed, pillows, and sleep posture to accommodate specific pain conditions, whether it’s using a body pillow for hip pain or sleeping in a reclined position for back pain.
Summary
Improving sleep in individuals with chronic pain is a multi-factorial process that requires addressing both the physical and psychological factors contributing to sleep disturbances. Chronic pain and poor sleep are intricately connected, and breaking this cycle involves managing pain, reducing anxiety and stress, and establishing healthy sleep habits. By incorporating strategies such as pain management techniques, cognitive behavioural therapy for insomnia, relaxation exercises, and optimizing the sleep environment, individuals with chronic pain can improve their sleep quality and overall well-being.
References
De La Rosa JS, Brady BR, Ibrahim MM, Herder KE, Wallace JS, Padilla AR, Vanderah TW. Co-occurrence of chronic pain and anxiety/depression symptoms in U.S. adults: prevalence, functional impacts, and opportunities. Pain. 2024 Mar 1;165(3):666-673. doi: 10.1097/j.pain.0000000000003056. Epub 2023 Sep 21. PMID: 37733475; PMCID: PMC10859853.
Kourbanova K, Alexandre C, Latremoliere A. Effect of sleep loss on pain-New conceptual and mechanistic avenues. Front Neurosci. 2022 Dec 20;16:1009902. doi: 10.3389/fnins.2022.1009902. PMID: 36605555; PMCID: PMC9807925.
Ulrich-Lai YM, Herman JP. Neural regulation of endocrine and autonomic stress responses. Nat Rev Neurosci. 2009 Jun;10(6):397-409. doi: 10.1038/nrn2647. PMID: 19469025; PMCID: PMC4240627.
Whale K, Gooberman-Hill R. The Importance of Sleep for People With Chronic Pain: Current Insights and Evidence. JBMR Plus. 2022 Jun 17;6(7):e10658. doi: 10.1002/jbm4.10658. PMID: 35866153; PMCID: PMC9289983.
Joon completed his Clinical Psychology training in New Zealand and has wide-ranging experience working in health, forensic and community settings across a number of different population groups. This has involved clinical roles in assessment and therapy, both as a lead clinician and as part of a wider multi-disciplinary team.