Part One
Aidan Rich, APA sports and exercise physiotherapist
Hip and knee osteoarthritis are very common conditions, affecting up to 5-15% of all people. Osteoarthritis can cause symptoms including pain, morning stiffness, loss of joint flexibility, swelling and reduced ability to undertake occupational and sporting activities.
There are a variety of treatment options available for treatment of hip and knee osteoarthritis, these are in three broad categories
Non-surgical (“conservative”) treatment
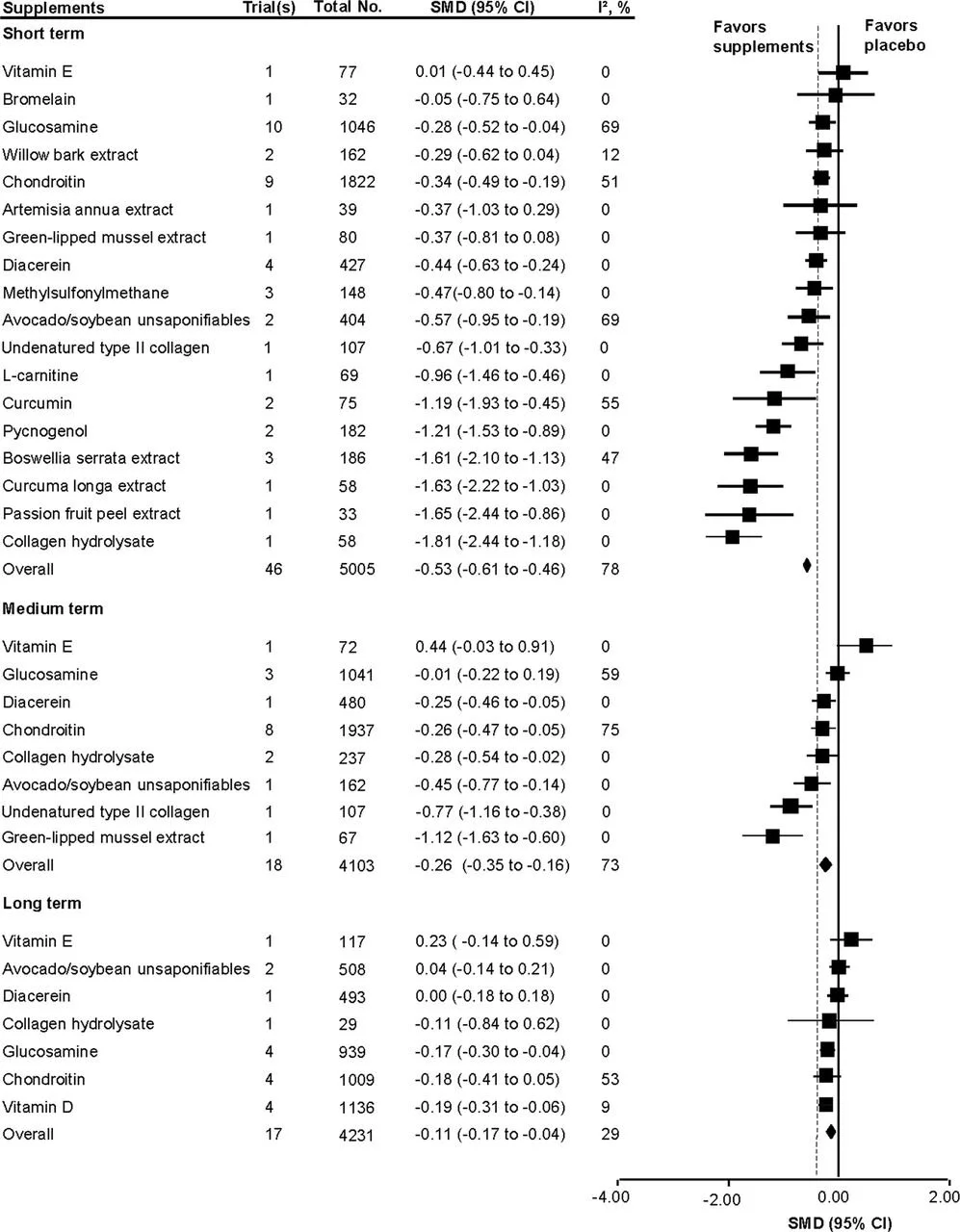
Supplements: There is a large number of supplements on the market with a lot of claims! The ones that have good evidence of benefit for knee and hip osteoarthritis include curcumin (from the spice tumeric) and green lipped mussel extract. These are a low risk, and potentially quite helpful option for knee and hip osteoarthritis and may be a consideration if you have this condition.
Passive treatments, such as massage, ultrasound, TENS: Most of us enjoy a good massage, me included! Massage is a safe treatment for knee osteoarthritis, and can provide good short-term (several weeks) benefits. Research suggests that the benefits are not maintained once treatment ceases.
TENS (Transcutaneous Electrical Nerve Stimulation) works by blocking some of the nociceptive (pain transmitting) fibres that relay the messages from your knee or hip back to your brain. Unfortunately there is limited evidence that TENS is more effective than placebo for knee osteoarthritis.
Ultrasound treatment was very common in physiotherapy practices in the 1990s and early 2000s, however it it used a lot less now. Research suggests it is no more effective than placebo ultrasound for knee osteoarthritis.
Exercise! This is such a big topic that I will expand on it below.
Injection therapies
PRP (Platelet Rich Plasma injections). PRP injections utilise a patient’s own blood, which is ‘spun’ in a centrifuge a a specific part injected. It has been quite controversial in the treatment of tendon conditions however the research is more supportive for knee osteoarthritis. A recent systematic review pooling injections into over 700 patients suggested that PRP is beneficial for up to 12 months for the treatment of pain and disability associated with knee osteoarthritis. There are limited studies looking at PRP in the treatment of hip osteoarthritis
PRP may be an option for treatment of knee osteoarthritis, particularly when other proven non-surgical options are already being undertaken. The downside of PRP is the cost, with most injections around the $400 mark in Melbourne.
Stem cells are a relatively new option for treating knee and hip osteoarthritis. The procedure involves harvesting cells from your abdomen, then growing up the culture and injecting it back into the knee or hip joint. It certainly isn’t cheap at around $10,000 per treatment! The governing body of the Australian General Practitioners Group (RACGP), has a ‘Strong Against’ position on stem cells for knee and hip osteoarthritis due to the lack of research supporting it’s use. The Australian Rheumatology Association has similar warnings against this treatment, suggesting it should only be used if part of a clinical trial and not marketed directly to patients. Proceed with caution!
Corticosteroid injections: There is some evidence showing that ‘cortisone’ injections may provide symptom relief in osteoarthritis for up to 6 months, however is limited research showing improvement beyond this time. Recent research has suggested that multiple injections may contribute to cartilage loss in the knee joint, which can accelerate the osteoarthritis process.
Surgical Intervention
Having surgery for any condition is obviously a big decision to make. Here are the main two options for surgical treatment for hip and knee osteoarthritis
Arthroscopy. Also known as ‘key hole surgery’, this is a procedure where the surgeon trims back any tears to the cartilage or meniscus in the knee joint. While this procedure was heralded as an effective treatment for knee osteoarthritis, a huge amount of research since 2002 has shown it to me no more effective than a placebo surgery. The Australian Knee Society (part of the Australian Orthopaedic Association) have recommended against knee arthroscopy in the cases of ‘routine’ knee osteoarthritis.
The effect of arthroscopy on hip osteoarthritis is less well understood (this is a much newer procedure) however a recent systematic review suggests that people with moderate or severe osteoarthritis are less likely to benefit
Joint replacement. This is the big one! In this procedure, the smooth lining of the hip and knee joint is replaced by metal (or ceramic or dense plastic) components. It’s also known as an ‘arthroplasty’ surgery.
Hip arthroplasty has had rapid advances over the last 15 years, with minimally invasive surgeries now available which allow the patient to be up and walking within 24 hours of surgery. There are no studies investigating placebo hip arthroplasty however results are generally quite good, with the majority of patients experiencing improvement in pain and function
Knee arthroplasty is generally seen as a larger procedure compared to hip arthroplasty. Again there are no placebo studies on this surgery, although many studies report a ‘failure rate’ (ongoing pain and disability) of around 20%. We do know some predictors of poor result of this surgery but these are not guarantees wither way.
Exercise is a big enough topic by itself so I’ve left it for another post, which you can find here.
Aidan Rich is an APA Sports and Exercise Physiotherapist at Advance Healthcare Boronia. He has an interest in all sports medicine conditions, and also runs GLA:D knee and hip osteoarthritis classes at the Boronia clinic.